While most patients aren’t aware of the difference between a Doctor of Osteopathy (DO) and a Medical Doctor (MD)—they simply see doctors as doctors—there has been a stigma within the medical community since the inception of osteopathic medicine by Dr. Andrew Taylor Still in 1874. Recent policy changes, evolving curriculum and certification/graduation criteria, and forward-moving trends in Graduate Medical Education (GME) match data reflect a culture shift from both sides. However, continued efforts must ensure the changes taking place are continually and fully executed.
As a partner in medical education, MedHub is actively working across the field to elevate awareness of the value of diverse pathways in healthcare professions, while also creating enhancements internally to optimize successful outcomes for osteopathic students and trainees.
Recently, we attended the Commission on Osteopathic College Accreditation (COCA) meeting where current Chair, Student Doctor Dominic J. Gigliotti, and Co-Chair, Student Doctor Josef Parra, from the Council of Osteopathic Student Government Presidents (COSGP), presented on the continuing challenges they and their peers still face today.
Keep reading to learn why collaboration between diverse medical education programs is critical, why challenges still exist, and efforts in progress to support the DO student, institution, and trainee.
MD or DO Degree: Different paths, same high standards
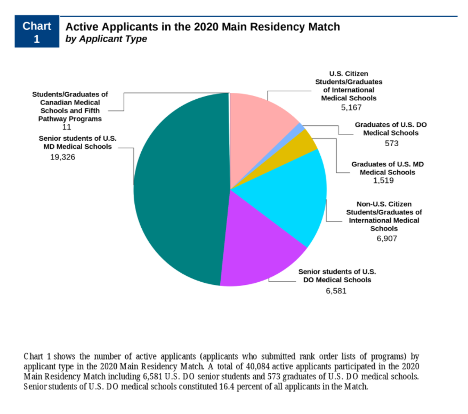
Upwards of 26,000 students graduate from medical schools in the United States each year. Roughly 25% are from medical education programs leading to a Doctor of Osteopathy (or DO) degree, with the remaining ~75% from medical education programs leading to a Medical Doctor (or MD) degree.
Although there are fewer Doctors of Osteopathy, the field of osteopathic medicine is growing tremendously. There are currently 135,000 osteopathic physicians—an 80% increase over the past decade.
The way MDs and DOs provide care is unique, but both have equally high standards that have led to the two educational paths to align at the GME level. In 2014, the Accreditation Council for Graduate Medical Education (ACGME), the American Osteopathic Association (AOA), and the American Association of Colleges of Osteopathic Medicine (AACOM) agreed to transition to a single accreditation system for GME by July 2020. That transition officially concluded on June 30, 2020.
The hope was that this shift would promote more collaboration in medical education, and that this collaboration would “better meet America’s healthcare needs for the 21st century.”
While philosophical differences exist between programs leading to a DO degree and those leading to an MD degree, similar high standards include:*
- Both require 4 years of medical school
- Both require a residency (GME) program that lasts 3-7 years
- Both are qualified to perform examinations, procedures, and prescribe medications
- Curriculum is rigorous and science-based in both fields, with the first two years focusing on the biomedical and clinical sciences
*Students pursuing a DO degree take the COMLEX-USA exam, while students pursuing an MD degree take the USMLE.
Although the transition has formally concluded, work is still being done to create full and complete alignment. The culture in the medical education community is still catching up from centuries of differences to ensure equal opportunities are realized for medical students, regardless of whether they are pursuing their MD or DO degree.
In August, the Coalition for Physician Accountability’s Undergraduate Medical Education-Graduate Medical Education Review Committee (UGRC) released their Recommendations for Comprehensive Improvement of the UME-GME Transition. One of those recommendations was to help mitigate structural bias by reporting comparable exams with different scales (COMLEX-USA and USMLE) within the electronic application system in a single field. This prevents an osteopathic student from being missed if a residency program filters based on USMLE score.
“I want to be evaluated on the same plane as any other applicant that applies to that residency program. I want you to evaluate me on my scores, I want you to evaluate me on my medical competency, and I want you to evaluate me on who I am as a person—not because of the letters I’m going to graduate with,” says Dominic Gigliotti, third-year DO student at the Alabama College of Osteopathic Medicine. Gigliotti is also the National Medical Education Representative of the Council of Osteopathic Student Government Presidents (COSGP), and recently presented at the Annual COCA Meeting.
Policy changes that promote the Osteopathic Doctor
Organizations like the COSGP and the American Osteopathic Association (AOA) regularly advocate for DO students through efforts that include:
- Ensuring educational institutions provide admissions opportunities to students pursing MD and DO degrees
- Discontinuing policies that allow for higher fees to be charged to osteopathic medical students for tuition, fees, and audition rotations
- Removing barriers to board certification
These initiatives have resulted in policy changes at individual institutions and sweeping updates like the AMA’s 2019 Equal Fees for Osteopathic and Allopathic Medical Students (H-295.876 .
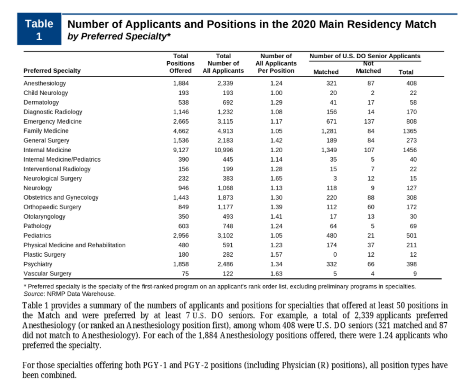
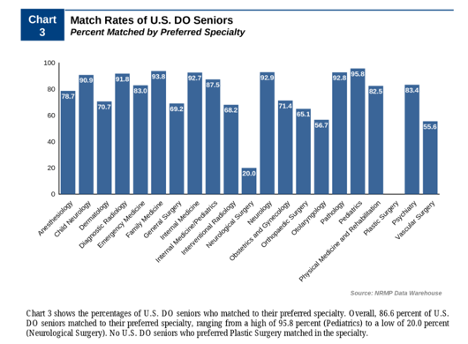
The momentum is moving in the right direction, as is indicated in the upward trend of Osteopathic students successfully attaining residency and fellowship positions at historically MD institutions. According to data from the National Resident Matching Program, 10 years ago, just 75% of DO seniors obtained postgraduate year one (PGY-1) positions in U.S. programs of graduate medical education (GME), while 94% of MD seniors were matched. In 2021, those percentages merged closer together at 89% and 93%, respectively.
References: Main Residency Match Data and Reports – The Match, National Resident Matching Program (nrmp.org)
Jose Parra, third-year DO student at Touro University Nevada and National Chair of the COSGP, says that there are still some technical issues that need to be sorted out to make the merger even more meaningful. For example, systems may not be set up to adequately assess the different board exams. “I think we all need to be more on a more level playing field and more on the same page,” he says.
Supporting all students, trainees, and medical institutions
As partners in medical education, MedHub advocates for growing awareness of diverse medical education pathways to ultimately make the healthcare community stronger. We are committed to staying current and engaged with the osteopathic community and will take the measures necessary to integrate changes to our processes, services and software platforms to be inclusive of both communities.
“It is critical we [MedHub] stay abreast of the evolving changes in policy, standards, and curriculum to ensure we are creating tools and services for all medical education and institutions regardless of foundation.” – Meggi Lensman, UME Consultant.
Below are the ways we are continuing to support this larger initiative for our clients.
Alignment in UME and GME solutions
We are bringing alignment to innovation and product initiatives for both medical education programs leading to an MD degree and DO degree, ensuring compliance and institutional oversight, and addressing their unique challenges with clinical placements and scheduling.
Adaptive training tools
The UME Learning Portal provides an interactive change management and systemic adoption tool that ensures inclusive osteopathic themes, foundations and terminology.
Learn more about the Learning Portal. >
Inclusive language
Through inclusive language and marketing, we are building awareness and addressing one medical community. This is a small, but important shift toward inclusion and cultural change.
Educated teams and support
We as a company stay abreast of the changing COCA and GME “Single Accreditation System” standards, and recognize the necessary cultural change needed to support our osteopathic students for successful match outcomes in competitive residency programs and specialties. We also understand the evolving policies in place by the AMA and AACOM to ensure equitable treatment for all students and trainees.
Our teams understand the osteopathic community’s unique challenges and specific language/terminology. We regularly discuss those challenges to address opportunities for integration in our software platforms as we move forward.
Thoughtful implementation
We understand how curriculum and the updated standards from COCA now require more central monitoring, enhanced research, updated curriculum and aligned topics of concentration. To bring this a step further, we have a UME and GME Consultant on hand during implementation to empower one medical community and conduct a business analysis during implementation, making note of uniformities for both fields of medicine, and their unique individual school and infrastructural challenges.
Learn more about our proven implementation process. >
Additional resources
Want to get involved or learn more about the efforts to remove the barriers faced by osteopathic students? The following organizations and resources are a great place to start.
- American Osteopathic Association (AOA)
- American Association of Colleges of Osteopathic Medicine (AACOM)
- AMA Equal Fees for Osteopathic and Allopathic Medical Students policy
- The DO advocacy news
- Single GME Accreditation System (SAS)
- The Coalition for Physician Accountability’s UME-GME Review Committee (UGRC) – 8/2021 Update